This guide aims to provide a structured approach to performing a newborn baby assessment in an OSCE setting. Check out the newborn baby assessment OSCE mark scheme here.
Background
The Newborn Infant Physical Examination (NIPE) must be performed within 72 hours of birth by a qualified practitioner.¹
The purpose of the examination of the newborn is:²
- To screen for abnormalities
- To make referrals for further tests or treatment as appropriate
- To provide reassurance to the parents
Where to perform the NIPE
The NIPE exam should be undertaken in a private area which provides confidentiality for parents when personal information is being discussed.
The room should be warm and well lit (preferably natural light, especially if jaundice is to be assessed).²
You’ll ideally require a changing mat to carry out the examination on.
Always make sure that the mother/parents are present for the newborn check, as an important part of the reason for the check is to answer queries and give reassurance.
Introduction
Wash hands:
- Hand hygiene is essential before and after the newborn check
- Always wash and use alcohol gel on your hands before examining the newborn
- Alcohol gel must dry completely before handling the newborn
Introduce yourself to the parents – state your name and role
Explain that you need to carry out a routine head to toe examination of their child.
Gain consent:
- Parents should have received the National Screening Committee leaflet ‘Screening tests for you and your baby’ in the antenatal period
- If the parent has not read the information booklet they must be given a copy to read before to the examination
- The aims and limitations of the examination should fully explained
Ask parent to undress the child down to their nappy.
Encourage the parents to ask questions during the check and to participate where appropriate.
The optimal way to perform the newborn check is by examining from head to toe sequentially.
Questions to ask the parents
Below are some key points you would ideally cover in a full assessment of a newborn baby. It should be noted however that in the context of an OSCE you are unlikely to be expected to cover all these history points due to time constraints.
- Maternal history:
- Pregnancy – date,time and type of delivery / complications/ high risk antenatal screening results
- Family history – hearing problems / hip dislocation / childhood heart problems
- Newborn history – feeding pattern / sleep pattern / urination / passing of meconium
Weight
Ensure that the baby’s weight is recorded and check on a weight chart whether the baby is:
- Small for dates (<10th centile)
- Appropriate weight for dates (10th-90th centile)
- Large for dates (>90th centile)
General inspection
Colour:
- Pallor
- Cyanosis
- Jaundice
- Rashes/erythema
Cry – note the volume (a weak cry may be an indicator the newborn is unwell)
Posture – note any gross abnormalities of posture (e.g. hemiparesis/Erb’s palsy)
Tone
Assess tone by gently moving the newborn’s limbs passively and observing the newborn when they’re picked up (your assessment of tone should continue throughout the examination).
The term “floppy infant syndrome” is used to describe abnormal limpness when an infant is born. Infants who suffer from hypotonia are often described as feeling and appearing as though they are “rag dolls”. Hypotonic infants often have difficulty feeding, as their mouth muscles cannot maintain a proper suck-swallow pattern, or a good breastfeeding latch.
Head
Size
Measure head circumference and record it in the baby’s notes.
Microcephaly is a medical condition in which the brain does not develop properly resulting in a smaller than normal head. Microcephaly may be present at birth or it may develop in the first few years of life.³
Macrocephaly is a condition in which the head is abnormally large; this includes the scalp, the cranial bone, and the contents of the cranium. Macrocephaly may be pathological, but many people with abnormally large heads or large skulls are healthy. Pathologic macrocephaly may be due to megalencephaly (enlarged brain), hydrocephalus (water on the brain), cranial hyperostosis (bone overgrowth), and other conditions.4
Shape
Inspect the shape of the head and note any abnormality.
Inspect the cranial sutures and note if they are closely applied, widely separated or normal.
Head moulding is common after birth and resolves within a few days.
Caput succedaneum is a neonatal condition involving a serosanguinous, subcutaneous, extraperiosteal fluid collection with poorly defined margins (often crossing suture lines) caused by the pressure of the presenting part of the scalp against the dilating cervix (tourniquet effect of the cervix) during delivery. Caput succedaneum does not usually cause complications and usually resolves over the first few days. 5
Cephalhaematoma is a firm swelling caused by haemorrhage between the skull and the periosteum secondary to rupture of blood vessels crossing the periosteum. Because the swelling is subperiosteal its boundaries are limited by the individual bones and therefore the swelling clinically will be noted not to cross suture lines (in contrast to a caput succedaneum). 6
Craniosynostosis is a condition in which one or more of the fibrous sutures in an infant skull prematurely fuses by turning into bone, thereby changing the growth pattern of the skull which can result in raised intracranial pressure and damage to intracranial structures. Surgical intervention is required with the primary goal being to allow normal cranial vault development to occur. This can be achieved by excision of the prematurely fused suture and correction of the associated skull deformities. 7
Fontanelle
Palpate the anterior fontanelle – note if it feels flat (normal), sunken or bulging (abnormal)
A tense bulging fontanelle may suggest raised ICP – e.g. hydrocephalus
A sunken fontanelle may suggest dehydration.
Skin
Colour – pallor / cyanosis / erythema / jaundice
Bruising / lacerations – may be secondary to trauma during childbirth
Facial birthmarks:
- Salmon patch
- Port wine stain
- Dry abrasions
Vernix – waxy or cheese-like white substance found coating the skin of newborn human babies (normal)
Other potential findings
Mongolian spot is a benign, flat, congenital birthmark with wavy borders and irregular shape. It is most commonly blue in colour and can be mistaken for a bruise. They normally disappears within 3-5 years after birth. 8
Naevus flammeus nuchae, often called stork bite or nevus simplex, is a congenital capillary malformation present in newborns. It is a common type of birthmark in a newborn and is usually temporary. 9
Milia are tiny white spots. They are blocked pores. About half of infants have milia on their face, most resolving within the first few weeks of life.
Capillary haemangiomas (“port wine stains”)
Toxic erythema of the newborn is a common and benign condition seen in newborn infants. It presents with various combinations of erythematous macules (flat red patches), papules (small bumps) and pustules. It is unusual for an individual lesion to persist for more than a day and the newborn is otherwise well throughout the episode.10
Neonatal jaundice can be physiological, appearing at 2-3 days and resolving by day 10. It can also be caused by a wide range of different pathologies including haemolytic disease, infection and Gilbert’s syndrome.
Face
Appearance – note any dysmorphic features
Asymmetry – e.g. facial nerve palsy
Trauma – likely to have occurred during labour (e.g. instrumental delivery)
Nose – patency of nasal passages
Eyes
Inspect the eyes for evidence of erythema or discharge (e.g. conjunctivitis).
Inspect the sclera by gently retracting the lower eyelid noting any discolouration (e.g. jaundice)
Position and size – inspect pupils for cataracts
Assess for red reflex:
- Use your ophthalmoscope to assess for red reflex
- An absent red reflex may suggest congenital cataracts or rarely neuroblastoma
Subconjunctival hemorrhages – these look dramatic but are benign, you should however document their presence
Ears
Inspect the pinna – asymmetry / prominence / accessory auricles
Note any skin tags
All infants should have a hearing screening test prior to discharge from hospital.
Mouth and palate
Clefts of hard or soft palate – directly observe and palpate
Tongue and gums – inspect for evidence of tongue-tie (ankyloglossia)
Neck and clavicles
Length of neck – e.g. abnormally short in Turner’s syndrome
Webbing of the neck – e.g. Turner’s syndrome
Neck swellings – e.g. Cystic hygroma
Clavicular fracture – secondary to traumatic birth (e.g. shoulder dystocia)
Upper limbs
Inspect for symmetry – ensure equal in size and length
Inspect fingers – ensure correct number and morphology
Inspect palms – should have two palmar creases on each hand
Palpate brachial pulses
Polydactyly is a congenital abnormality where there are supernumerary fingers or toes.
A single palmar crease is associated with Down’s syndrome.
Chest
Inspect
Chest wall deformities (e.g. pectus excavatum)
Chest wall expansion – asymmetry may be noted unilateral lung pathology (e.g. pneumonia)
Lungs
Note any respiratory distress (e.g. intercostal recession) – normal respiratory rate is 30-60 in newborns
Auscultate the lungs:
- Auscultate to ensure there is air entry bilaterally
- Listen for any added sounds – wheeze / crackles / grunting
Heart
Auscultate the heart:
- Use a paediatric stethoscope
- Normal heart rate is around 120-150 bpm
- Listen for any added sounds (murmurs)
- If a murmur is noted, try to identify where it is heard loudest and if it radiates anywhere
Abdomen
Inspect for evidence of abdominal distension
Inspect for evidence of any inguinal hernias – will need paediatric surgical review
Palpate the abdomen:
- Liver – should be no more than 2cm below costal margin
- Spleen – should not be palpable
- Kidneys – only palpable on deep bimanual palpation
- Bladder – should not be palpable
Umbilicus
Inspect for any discharge or hernias
Note any offensive smell – may suggest infection
Genitalia
Note any ambiguity of genitalia – e.g. congenital adrenal hyperplasia
Males:
- Normal prepuce (exclude hypospadia)
- Normal urinary stream – (should be observed by 24 hrs – dribbling suggests posterior urethral valves)
- Hydroceles – collection of fluid in the scrotum – transilluminates
- Palpate scrotum to ensure both testes are present – absence suggests they may be undescended
Females:
- Inspect labia – ensure they not be fused
- Inspect clitoris – ensure it is normal size
- Vaginal discharge – white discharge is normal due to maternal oestrogens
Lower limbs
Inspect limb symmetry – should be equal in size and length
Assess tone in both lower limbs
Assess movement in both lower limbs
Palpate femoral pulses
Assess for oedema
Assess knees – hyper-extensile/dislocatable
Ankle deformities – e.g. talipes
Ensure correct number of digits on each foot
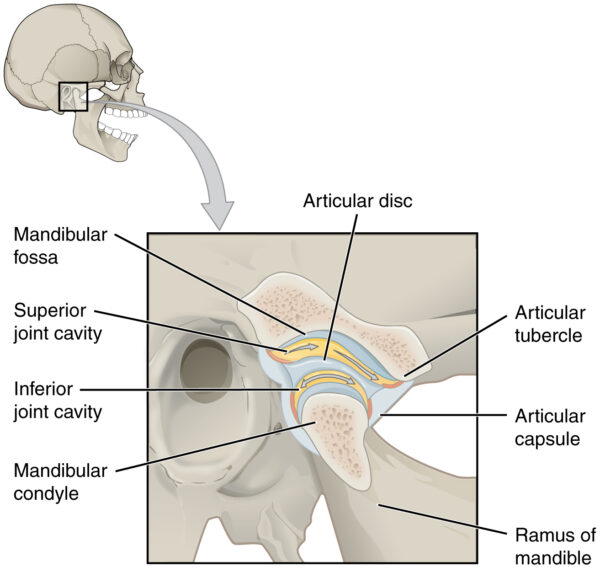
Hips
Barlow’s and Ortolani’s test are carried out as part of the routine newborn examination to detect hip joint instability and dislocation. Although both legs can be assessed at the same time, it is optimal to stabilize the pelvis with one hand and manipulate one leg at a time.11
Barlow’s test
1. Barlow’s test is performed by adducting the hip (bringing the thigh towards the midline) whilst applying light pressure on the knee with your thumb, directing the force posteriorly. 12
If the hip is unstable, the femoral head will slip over the posterior rim of the acetabulum, producing a palpable sensation of subluxation or dislocation.
If the hip is dislocatable the test is considered positive. The Ortolani maneuver is then used to confirm the positive finding (i.e. that the hip actually dislocated).
Ortolani’s test
Ortolani’s test is used to confirm posterior dislocation of the hip joint.13
1. Flex the hips and knees of a supine infant to 90 degrees
2. Then with your index fingers placing anterior pressure on the greater trochanters, gently and smoothly abduct the infant’s legs using your thumbs
A positive sign is a distinctive ‘clunk’ which can be heard and felt as the femoral head relocates anteriorly into the acetabulum.
This tests assesses specifically for posterior dislocation of the hip.
Back and spine
Inspect the spine for:
- Scoliosis
- Hair tufts
- Naevus
- Abnormal skin patches
- Birthmarks
- Sacral pits
Hair tufts and sacral pits can be associated with underlying neural tube defects (spina bifida).
Anus
Inspect the anus for patency
Meconium should be passed within 24 hours
Reflexes
Assess the newborn’s reflexes
Palmar grasp reflex is a primitive reflex. It appears as early as 16 weeks in utero and persists until five or six months of age. When an object is placed in the infant’s hand and strokes their palm, the fingers will close and they will grasp it with a palmar grasp.14
Sucking reflex – causes the child to instinctively suck anything that touches the roof of their mouth, and simulates the way a child naturally eats.
Rooting reflex – present at birth and disappears around four months of age, as it gradually comes under voluntary control. The rooting reflex assists in the act of breastfeeding. A newborn infant will turn its head toward anything that strokes its cheek or mouth, searching for the object by moving its head in steadily decreasing arcs until the object is found.15
Stepping reflex – present at birth, though infants this young cannot support their own weight. When the soles of their feet touch a flat surface they will attempt to walk by placing one foot in front of the other. This reflex disappears at six weeks due to an increased ratio of leg weight to strength. It reappears as a voluntary behavior around eight months to one year old. 16
Moro reflex – present at birth, peaks in the first month of life, and begins to disappear around 2 months of age. It is likely to occur if the infant’s head suddenly shifts position, the temperature changes abruptly, or they are startled by a sudden noise. The legs and head extend while the arms jerk up and out with the palms up and thumbs flexed. Shortly afterward the arms are brought together and the hands clench into fists, and the infant cries loudly.17
To complete the examination…
Share the results of the assessment with the parents, explaining the reason for any referrals you feel are required
Ask if the parents have any further questions
Thank the parents
Offer to dress the baby or allow parents to do so (depending on their preference)
Wash hands
Document your findings and suggest any relevant investigations or referrals
References
Click to show
1. Newborn and Infant Physical Examination Screening Programme Handbook 2016/17. Public Health England. Published April 2016.Retrieved 15 March 2017.
2. Newborn Infant Physical Examination. Nottingham Neonatal Service – Clinical Guidelines. Published November 2015. Retrieved 15 March 2017.
3. “NINDS Microcephaly Information Page”. NINDS. June 30, 2015. Retrieved 15 March 2017.
4. Williams CA, Dagli A, Battaglia A (2008). “Genetic disorders associated with macrocephaly”. Am J Med Genet A. 146A (16): 2023–37. doi:10.1002/ajmg.a.32434. PMID 18629877. Retrieved 15 March 2017.
5. Diane Fraser (9 April 2009). Myles’ Textbook for Midwives. Elsevier Health Sciences. p. 860. ISBN 978-0-443-06939-0. Retrieved 15 March 2017.
6.“Cephalohematoma“. Wikipedia. N.p., 2017. Retrieved 15 March 2017.
7. Slater BJ, Lenton KA, Kwan MD, Gupta DM, Wan DC, Longaker MT (April 2008). “Cranial sutures: a brief review”. Plast. Reconstr. Surg. 121 (4): 170e–8e. doi:10.1097/01.prs.0000304441.99483.97. PMID 18349596.
8. Circumscribed dermal melanosis (Mongolian spot)(1981) Kikuchi I, Inoue S. in “Biology and Diseases of Dermal Pigmentation”, University of Tokyo Press , p83
9. James, William; Berger, Timothy; Elston, Dirk (2005). Andrews’ Diseases of the Skin: Clinical Dermatology. (10th ed.). Saunders. Page 169. ISBN 0-7216-2921-0.
10.“Toxic Erythema Of The Newborn | Dermnet New Zealand“. Dermnetnz.org. Published 2012. Retrieved 15 March 2017.
11. American Academy of Pediatrics. Clinical Practice Guideline: early detection of developmental dysplasia of the hip. Pediatrics. 2000;105:896-905.
12. French LM, Dietz FR (July 1999). “Screening for developmental dysplasia of the hip”. American Family Physician. 60 (1): 177–84, 187–8. PMID 10414637.
13. Storer SK, Skaggs DL (October 2006). “Developmental dysplasia of the hip”. American Family Physician. 74 (8): 1310–6. PMID 17087424.
14. Jakobovits, AA (2009). “Grasping activity in utero: a significant indicator of fetal behavior (the role of the grasping reflex in fetal ethology).”. Journal of perinatal medicine. 37 (5): 571–2. doi:10.1515/JPM.2009.094. PMID 19492927.
15. Odent M. The early expression of the rooting reflex. Proceedings of the 5th International Congress of Psychosomatic Obstetrics and Gynaecology, Rome 1977. London: Academic Press, 1977: 1117-19.
16. Siegler, R.; Deloache, J.; Eisenberg, N. (2006). How Children Develop. New York: Worth Publishers. p. 188. ISBN 978-0-7167-9527-8.
17. Rauch, Daniel (2006-10-05). “MedlinePlus Medical Encyclopedia: Moro Reflex”. Retrieved 15 March 2017.