Chest x-rays (CXR) are a frequently performed radiological investigation that you’ll be expected to be capable of interpreting (as due to the sheer volume of chest x-rays requested they are often not reported immediately). Therefore before hitting the wards as foundation doctors it is essential that you develop the ability to interpret chest x-rays, of particular importance is the ability to recognise findings that require immediate medical attention.
Confirm details
Always begin by checking the following:
- Patient details (name / DOB)
- Date & time the film was taken
- Any previous imaging (useful for comparison)
Assess image quality
Then briefly assess the quality of the image: A mnemonic you may find useful is ‘RIPE’:
- Rotation – the medial aspect of each clavicle should be equidistant from the spinous processes.
- Inspiration – 5-6 anterior ribs, the lung apices, both costophrenic angles and lateral rib edges should be visible.
- Projection – AP vs PA film.
- Exposure – left hemidiaphragm visible to the spine and vertebrae visible behind heart.
CXR interpretation (ABCDE approach)
Airway
Trachea
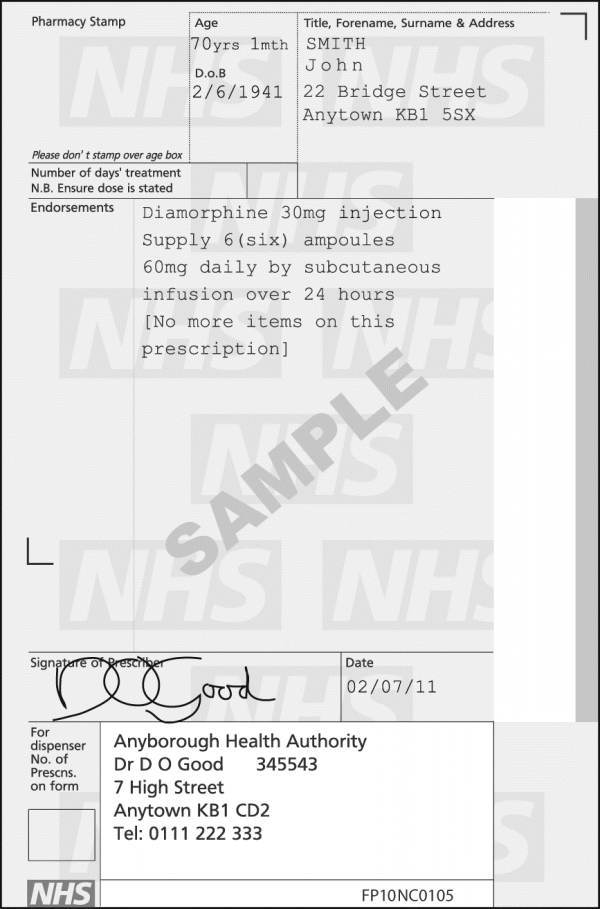
Is the trachea significantly deviated?
- The trachea is normally located centrally or just slightly off to the right
- If the trachea is deviated, look for anything that could be pushing or pulling at the trachea.
- Also inspect for any paratracheal masses / lymphadenopathy
Pushing of trachea – e.g. large pleural effusion / tension pneumothorax
Pulling of trachea – e.g. consolidation with lobar collapse
Rotation of the patient can give the appearance of a deviated trachea, so as mentioned above, check the clavicles to rule out rotation as the cause.
![Pleural effusion with tracheal deviation 2]()
Pleural effusion with tracheal deviation 2
Carina and Bronchi
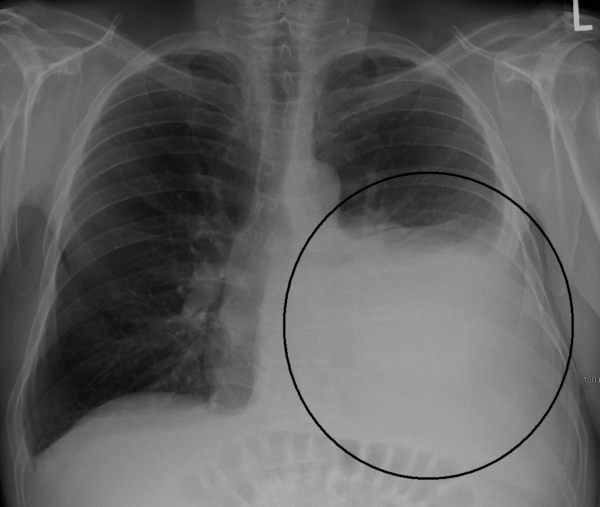
The carina is located at the point at which the trachea divides into the left and right main bronchus.
On a good quality CXR this division should be visible and is an important landmark when assessing nasogastric tube placement, as the NG tube should dissect the carina if it is correctly placed (i.e. not in the airway).
The right main bronchus is generally wider, shorter and more vertical than the left main bronchus. As a result it is more common for inhaled foreign objects to become lodged here (as the route is more direct).
Depending on the quality of the CXR you may be able to see the main bronchi branching into further subdivisions of bronchi which supply each of the lungs lobes.
![Carina & Bronchi (Normal CXR)]()
Carina & Bronchi (Normal CXR)
Hilar structures
- The hilar consist of the main pulmonary vasculature and the major bronchi.
- Each hilar also has a collection of lymph nodes which aren’t usually visible in healthy individuals.
- The left hilum is often positioned slightly higher than the right, but there is a wide degree of variability between individuals.
- The hilar are usually the same size, so asymmetry should raise suspicion of pathology.
Hilar enlargement can be caused by a number of different pathologies:
- Bilateral symmetrical enlargement is typically associated with sarcoidosis.
- Unilateral / asymmetrical enlargement may be due to underlying malignancy.
Abnormal hilar position can also be due to a range of different pathologies. You should (as with the trachea) look for any evidence of the hilar being pushed (e.g. by an enlarging soft tissue mass) or pulled (e.g. lobar collapse).
Breathing
Lung fields
Inspect the lung fields:
- When looking at a CXR we divide each of the lungs into 3 zones, each occupying 1/3 of the height of the lung.
- These zones do not equate to lung lobes (e.g. the left lung has 3 zones but only 2 lobes).
- Inspect each of the zones of the lung first ensuring that lung markings occupy the entire zone.
- Compare each zone between lungs, paying close attention for any asymmetry (some asymmetry is normal and caused by the presence of various anatomical structures e.g. the heart).
- Some lung pathology causes symmetrical changes in the lung fields, which can make it more difficult to recognise, so it’s important to keep this in mind (e.g. pulmonary oedema).
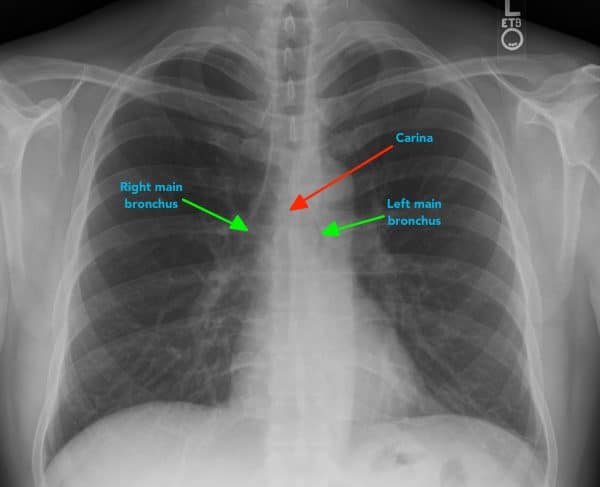
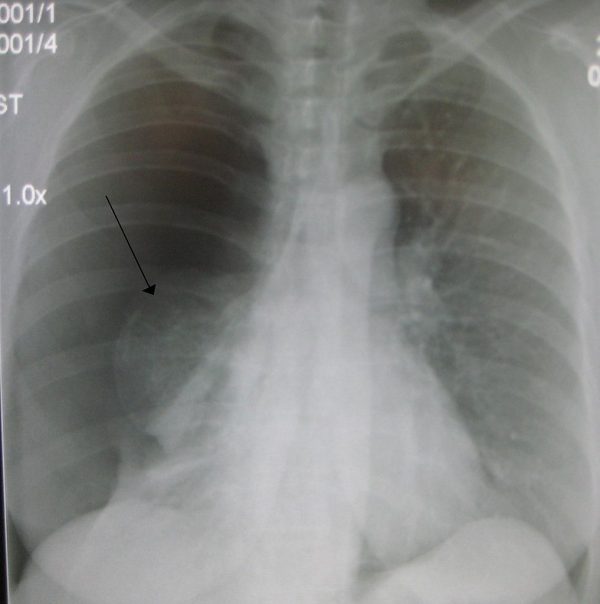
Increased density in a given area of the lung field may suggest pathology (e.g. consolidation / malignant lesion).
The complete absence of lung markings within a segment of the lung field should raise suspicion of pneumothorax.
![Lung tumour]()
![Right sided pneumonia1]()
Pleura
Inspect the pleura:
- The pleura are not normally visible in healthy individuals.
- Inspect the borders of each of the lungs to ensure lung markings extend all the way to the edges of the lung fields (if there appears to be an area lacking lung markings with decreased density this may suggest the presence of a pneumothorax).
- Fluid (hydrothorax) or blood (haemothorax) can also accumulate in the pleural space, causing an area of increased opacity.
If a pneumothorax is suspected, you should reassess the trachea for evidence of deviation away from the pneumothorax which is in keeping with a tension pneumothorax. This is a medical emergency requiring immediate intervention. If a tension pneumothorax is suspected clinically (shortness of breath and tracheal deviation) then immediate intervention should be performed without waiting for imaging as this condition will result in death if left untreated.
Pleural thickening can be caused by mesothelioma.
![Right sided pneumothorax]()
![Pleural thickening in the context of mesothelioma2]()
Cardiac
Assess heart size
In a healthy individual the heart should occupy no more than 50% of the thoracic width (e.g. a cardiothoracic ratio of <0.5).
This rule only applies to PA chest x-rays (as AP films exaggerate heart size), so you should not draw any conclusions about heart size from an AP film.
If the heart occupies more than 50% of the thoracic width (on a PA CXR) then this suggests abnormal enlargement (cardiomegaly). Cardiomegaly can occur for a wide variety of reasons including valvular disease, cardiomyopathy, pulmonary hypertension and pericardial effusion.
Assess heart borders
Inspect the borders of the heart which should be well defined in healthy individuals:
- The right atrium makes up most of the right heart border.
- The left ventricle makes up most of the left heart border.
The heart borders may become difficult to distinguish from the lung fields as a result of various pathological processes (e.g. consolidation) which cause increased opacity of the lung tissue.
- Loss of definition of the right heart border is associated with right middle lobe consolidation
- Loss of definition of the left heart border is associated with lingular consolidation
![Cardiomegaly]()
Cardiomegaly2
Diaphragm
The right hemi-diaphragm is in most cases higher than the left in healthy individuals (as a result of the underlying liver). The stomach underlies the left hemi-diaphragm and is best identified by the gastric bubble located within it.
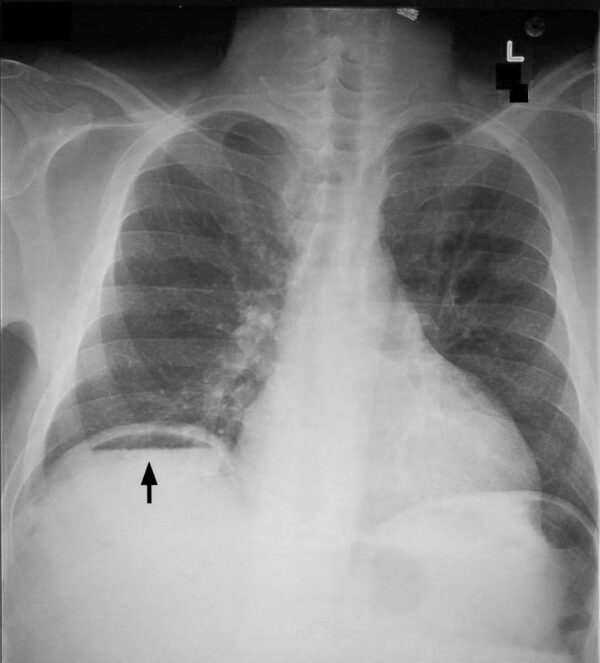
The diaphragm should be indistinguishable from the underlying liver in healthy individuals on an erect CXR, however if free gas is present as a result of bowel perforation air accumulates under the diaphragm causing it to lift and become visibly separate from the liver. If you see free gas under the diaphragm it indicates the need for urgent senior review as further imaging such as CT will likely be required to identify the source of free gas.
![Pneumoperitoneum3]()
Pneumoperitoneum3
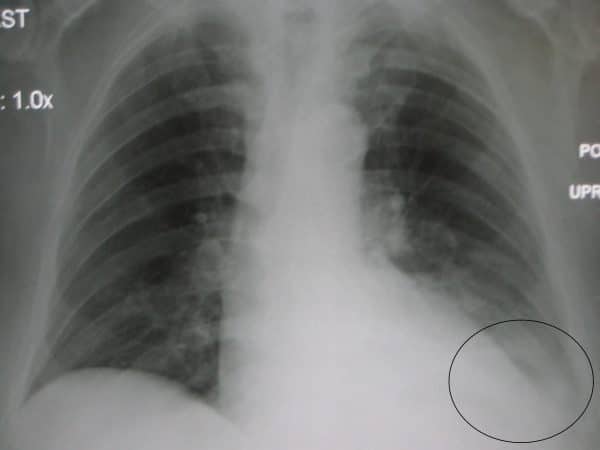
Costophrenic angles
The costophrenic angles are formed from the dome of each hemi-diaphragm and the lateral chest wall.
In a healthy individual the costo-phrenic angles should be clearly visible on a normal CXR as a well defined acute angle.
Loss of this acute angle (sometimes referred to as costophrenic blunting) can suggest the presence of fluid or consolidation in the area. Costophrenic blunting can also occur secondary to lung hyperinflation (seen in diseases such as COPD) as a result of diaphragmatic flattening and subsequent loss of the acute angle.
![Costophrenic blunting secondary to pneumonia2]()
Costophrenic blunting secondary to pneumonia2
Everything else
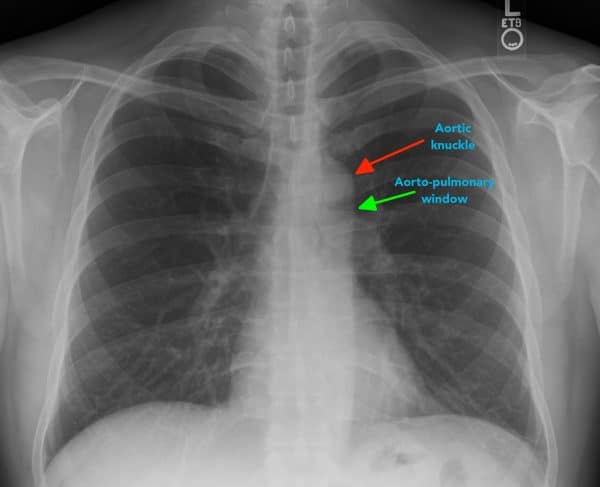
Mediastinal contours
The mediastinum contains the heart, great vessels, lymphoid tissue and a number of potential spaces where pathology can occur. The exact boundaries of the mediastinum aren’t particularly visible on a CXR, however there are some important structures that you should assess.
Aortic knuckle:
- Left lateral edge of the aorta as it arches back over the left main bronchus.
- Loss of definition of the aortic knuckles contours can be caused by an aneurysm.
Aorto-pulmonary window:
- The aorto-pulmonary window is a space located between the arch of the aorta and the pulmonary arteries.
- This space can be lost as a result of mediastinal lymphadenopathy (e.g. malignancy).
![Aortic knuckle & Aortopulmonary window]()
Aortic knuckle & Aortopulmonary window
Bones
Inspect the visible skeletal structures looking for any abnormalities (e.g. fractures / lytic lesions).
Soft tissues
Inspect the soft tissues for any obvious abnormalities (e.g. large haematoma).
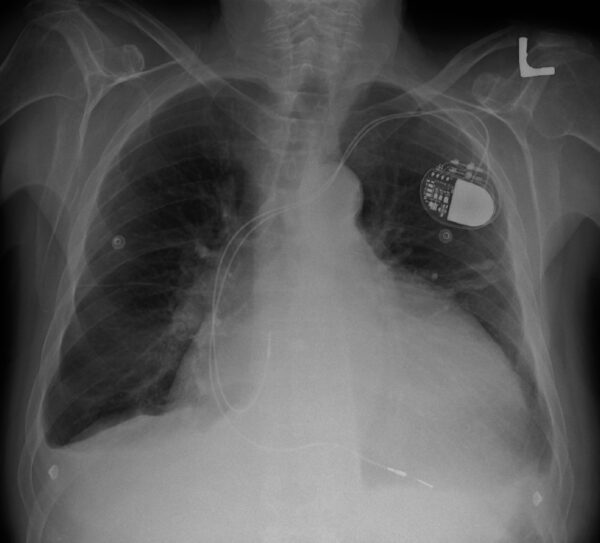
Tubes / Valves / Pacemakers
Lines (e.g. central line / ECG cables).
Artificial valves (e.g. aortic valve replacement).
Pacemaker (often located below the left clavicle).
References
- By James Heilman, MD (Own work) [CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0) or GFDL (http://www.gnu.org/copyleft/fdl.html)], via Wikimedia Commons
- By James Heilman, MD – Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=14634441
- By Clinical_Cases: I made the photo myself, licensed under Creative Commons license. – Modification of http://en.wikipedia.org/wiki/Image:Pneumoperitoneum.jpg Image source: http://clinicalcases.blogspot.com/2004/03/bloody-ascites-and-gas-under-diaphragm.html, CC BY-SA 2.5, https://commons.wikimedia.org/w/index.php?curid=2294165
- By Mikael Häggström, CC0, https://commons.wikimedia.org/w/index.php?curid=15228530